

What causes hidradenitis suppurativa (HS)?
While genetics and environment are among the factors that play a role in the development of HS, the exact cause of the condition is still unknown. HS is a lot more than just what you can see and feel on the outside. In fact, it’s believed to be related to a problem in the immune system. That’s why people sometimes use the term “autoimmune disease” to describe HS—though research has shown it's actually a systemic inflammatory condition related to the immune system.
While there are many things still not understood about HS, let’s take a deeper look at what medical research has uncovered. Watch the video below for an inside look at HS:
Looking at HS beneath the surface
To better understand HS, let’s go from the inside, out—starting with the immune system.
Business as usual
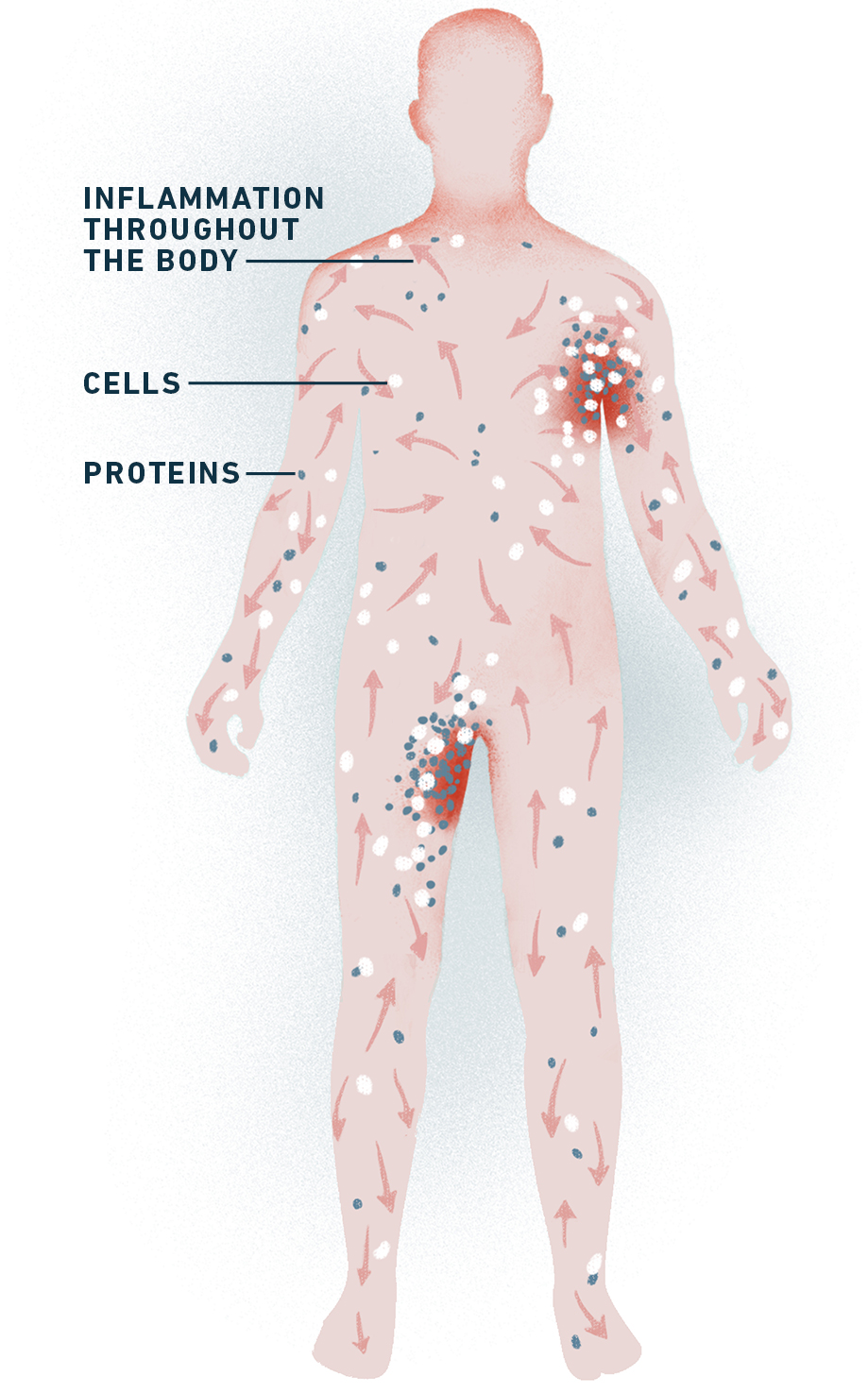
Picture your immune system operating like a network of factories throughout your body. It produces highly specified proteins and cells that fight off harmful germs and bacteria and help you recover from injuries like broken bones, bruises, or sprains.
When your immune system is healthy, these cells and proteins usually stay at normal levels. But when they come across trouble in your body, the factories get a signal to crank up production.
This sudden, temporary increase in cells and proteins causes inflammation to happen. This is a natural reaction in your body and helps your body to heal. Once the problem is dealt with, another signal goes out to resume normal production.
A snag in the system
For people with HS, the signal to create inflammation is uncontrolled, producing too many cells and proteins throughout the body for too long. Even when you’re not seeing or feeling a painful flare at the skin level, your immune system is overactive—making it more likely you’ll experience flares in the future.
The consequences of HS’s uncontrolled inflammation starts on the inside—before showing up in the layers of the skin as nodules, abscesses, and tunnels. And even when these symptoms seem to have moved away from a certain area of the skin, they can leave deep, permanent scars.
Like in HS, people with other chronic diseases (like rheumatoid arthritis, Crohn’s disease, and ulcerative colitis) can have increased inflammation from their immune system. It just impacts other areas of their body. HS is not thought to cause these diseases or vice versa. It’s important to tell your doctor if you are experiencing signs or symptoms of other diseases. Learn more about HS comorbidities.
The bottom line
Once you understand the science behind HS, you can easily see how this condition is nobody’s fault—especially your own. The good news is that medical research has been growing rapidly in recent years—with many strides being made in the understanding of HS and how to care for it.
So, what can you do about it?
Now that you are aware of the important role systemic inflammation plays, a candid conversation with your dermatologist can help you determine the most appropriate plan for managing your HS.
Recommended for you:

